As COVID-19 ravages healthcare systems worldwide, cases of infection among patients with systemic lupus erythematosus (SLE) are increasingly reported. While there had been 2 reports on incident hospitalized cases from the US and France,1,2 there have been no reports of SLE patients with COVID-19 infection from the Asia Pacific region.
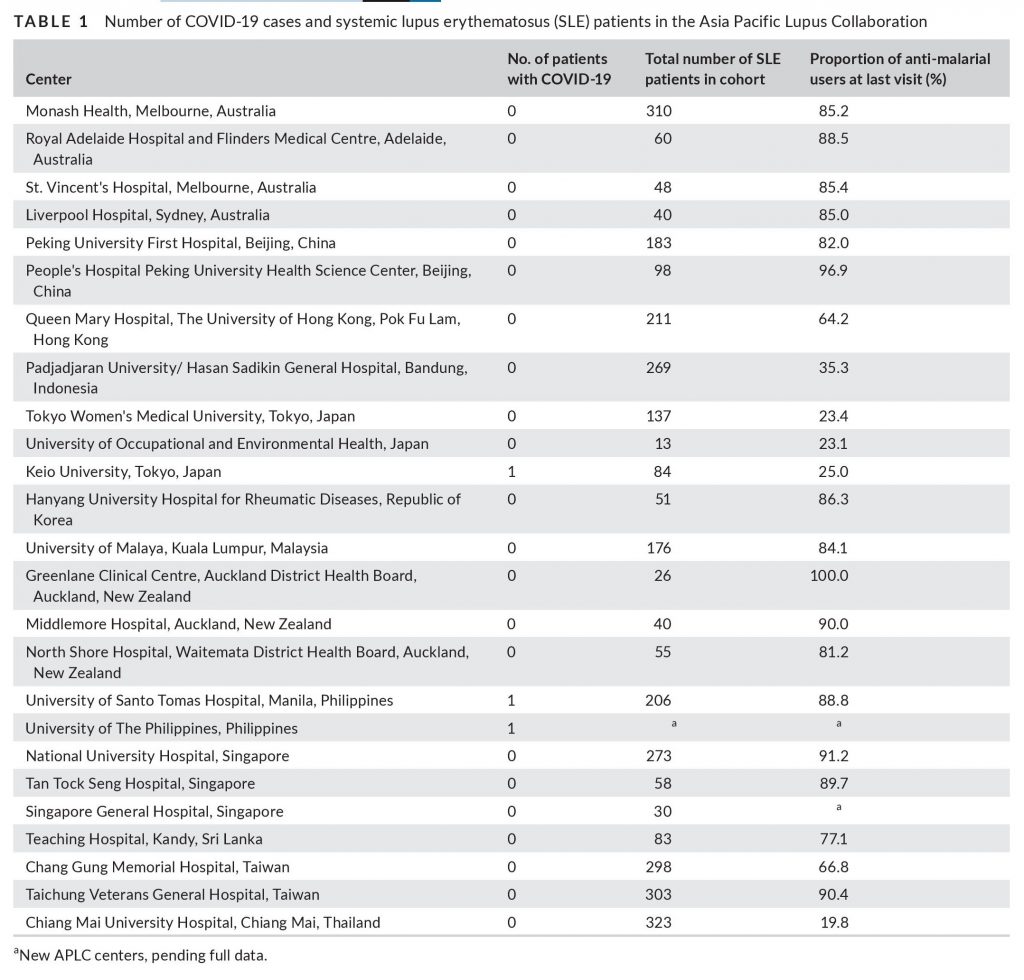
The Asia Pacific Lupus Collaboration (APLC) patient cohort comprises 3375 patients from 25 centers in Australia, China, Hong Kong, Indonesia Japan, Korea, Malaysia, New Zealand, Philippines, Singapore, Sri Lanka, Taiwan, Thailand.3 On 3 June, principal investigators of APLC centers were asked to respond to a brief email questionnaire regarding current or historical COVID-19 cases in their cohorts. Patients and the public were not involved in the conduct of this research. Table 1 describes the number of COVID-19 patients, number of SLE patients and the prevalence of hydroxychloroquine use. In total, only 3 cases of COVID-19 were reported. Here, we briefly describe their clinical course.
Patient 1 was a 58-year-old Japanese woman with stable SLE, maintained on prednisolone monotherapy (5 mg daily) without hydroxychloroquine. Her daughter was diagnosed with COVID-19 infection and the patient was found to be positive for SARS-CoV-2 on screening. Although she was asymptomatic, her clinical course was complicated by severe thrombocytopenia (nadir 5 × 109 /L) which required intravenous immunoglobulin and prednisolone 20 mg daily. The thrombocytopenia was attributed to SLE flare as its severity was assessed to be out of proportion to her asymptomatic COVID-19 infection. In addition, hypocomplementemia was observed. Platelet count eventually improved and she was discharged.
Patient 2 was a 32-year-old Filipino woman with active lupus nephritis who was treated with hydroxychloroquine, mycophenolate mofetil and prednisolone 30 mg daily. She resided 5 hours away from her lupus center and had a history of poor treatment adherence. During the pandemic, only phone consultations were performed, during one of which she informed her rheumatologist that she had been initiated on hemodialysis at a local hospital for deteriorating renal function. Subsequently, her rheumatologist was informed that she had passed away from COVID-19 pneumonia at the provincial hospital. Details surrounding her COVID-19 infection were not accessible.
Patient 3 was a 29-year-old Filipino woman with SLE (on hydroxychloroquine, azathioprine and low-dose prednisolone), hypertensive heart disease and chronic kidney disease who presented with bilateral COVID-19 pneumonia and peripheral edema. Concurrently, she was found to have active lupus nephritis which required increase in prednisolone to 50 mg daily. She was discharged when pneumonia and lupus nephritis improved.
In summary, we report three cases of COVID-19 infection in SLE patients from the Asia Pacific, of which one was fatal. Notably, all three patients had active SLE which required escalation of treatment just before, or during treatment for COVID-19 infection, in contrast to reports from France.2 Importantly, patient 2 could not directly access her rheumatologist during the pandemic and only phone consultations were used. Further research on the impact of reduced care access and the utility of alternative care models, such as teleconsultation, is needed for patients with SLE.
While the incidence of COVID-19 in SLE is unknown, 16 (4%) of the 450 patients in the Colombia Lupus Cohort developed symptomatic COVID-19 infection.1 Based on a report censored on 15 April in Hong Kong, none of the 1016 COVID-19 cases had a history of SLE.4 In this report, we describe only 3 cases identified among our 3375 SLE patients. Although we did not systematically capture infection rates in a protocolized manner, the low number of COVID-19 infections, at ~ 0.1% of the APLC cohort, does not suggest a major burden of COVID-19 among SLE patients. Possible reasons accounting for this included the low background prevalence of COVID-19 in the region compared with other parts of the world at the time of the report and increased measures taken by SLE patients to avoid infections. We eagerly await data from other SLE cohorts.
CONFLICT OF INTEREST
The authors declare no competing interests.
AUTHOR CONTRIBUTIONS
AL, RKR, EM and CJC contributed to the conception or design of the work. All authors contributed to the acquisition, analysis and interpretation of data. CJC, RKR and AL drafted the work. All coauthors revised it critically for important intellectual content. Final approval of the version published was obtained from all authors. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
ETHICS APPROVAL
Principal Investigators of individual centers obtained valid written informed consent in accordance with local authority regarding ethical conduct of human research, which conformed to the provisions of the Declaration of Helsinki. In addition, Monash University ethics approval has been obtained to store the pooled database, perform analyses and subsequently publish the findings.
Jiacai Cho 1
Rangi Kandane-Rathnayake 2
Worawit Louthrenoo 3
Alberta Hoi 2
Vera Golder 2
Yi-Hsing Chen 4
Shue Fen Luo 5
Yeong-Jian Jan Wu 5
Laniyati Hamijoyo 6
Chak Sing Lau 7
Sandra Navarra 8
Leonid Zamora 8
Michael Tee 9
Angelito Flora Jr 9
Zhan-Guo Li 10
Yuan An 10
Sargunan Sockalingam 11
Yasuhiro Katsumata 12
Masayoshi Harigai 12
Yanjie Hao 13
Zhuoli Zhang 13
Jun Kikuchi 14
Tsutomu Takeuchi 14
Duminda Basnayake 15
Fiona Goldblatt 16
Madelynn Chan 17
Kristine (Pek Ling) Ng 18
Sang-Cheol Bae 19
Shereen Oon 20
Sean O’Neill 21
Kathy Gibson 21
Sunil Kumar 22
Annie Hui Nee Law 23
Nicola Tugnet 24
Yoshiya Tanaka 25
Mandy Nikpour 20
Eric Morand 2
Aisha Lateef 1
1 National University Hospital, Singapore, Singapore
2 Monash University, Melbourne, Australia
3 Chiang Mai University Hospital, Chiang Mai, Thailand
4 Taichung Veterans General Hospital, Taichung, Taiwan
5 Chang Gung Memorial Hospital, Taoyuan, Taiwan
6 Padjadjaran University/Hasan Sadikin General Hospital, Bandung, Indonesia
7 The University of Hong Kong, Hong Kong, China
8 University of Santo Tomas Hospital, Manila, Philippines
9 University of the Philippines, Manila, Philippines
10 People’s Hospital, Peking University Health Science Center, Beijing, China
11 University of Malaya, Kuala Lumpur, Malaysia
12 Tokyo Women’s Medical University, Shinjuku-ku, Japan
13 Peking University First Hospital, Beijing, China
14 Keio University, Minato-ku, Japan
15 Teaching Hospital, Kandy, Sri Lanka
16 Royal Adelaide Hospital And Flinders Medical Centre, Adelaide, Australia
17 Tan Tock Seng Hospital, Singapore, Singapore
18 North Shore Hospital, Waitemata District Health Board, Auckland, New Zealand
19 Hanyang University Hospital for Rheumatic Diseases, Seongdong-gu, Republic of Korea
20 St. Vincent’s Hospital, Melbourne, Australia
21 Liverpool Hospital, Sydney, Australia
22 Middlemore Hospital, Auckland, New Zealand
23 Singapore General Hospital, Singapore, Singapore
24 Auckland District Health Board, Auckland, New Zealand
25 University of Occupational and Environmental Health, Kitakyushu, Japan
Correspondence
Jiacai Cho, National University Hospital, 1E, Kent Ridge
Road, Singapore 119228, Singapore.
Email: [email protected]
REFERENCES
1. Gartshteyn Y, Askanase AD, Schmidt NM, et al. COVID-19 and systemic lupus erythematosus: a case series. Lancet Rheumatol. 2020.
https://doi.org/10.1016/S2665-9913(20)30161-2
2. Mathian A, Mahevas M, Rohmer J, et al. Clinical course of coronavirus disease 2019 (COVID-19) in a series of 17 patients with systemic lupus erythematosus under long-term treatment with hydroxychloroquine. Ann Rheum Dis. 2020;79(6):837-839.
3. Kandane-Rathnayake R, Golder V, Louthrenoo W, et al. Development
of the Asia Pacific Lupus Collaboration cohort. Int J Rheum Dis.
2019;22(3):425-433.
4. So H, Mak JWY, Tam L-S. No SLE with COVID-19 in Hong Kong: the
effect of masking? J Rheumatol. 2020;47. https://doi.org/10.3899/
jrheum.200605
![]()